TURP (Transurethral Resection of Prostate)
Key Points
TURP stands for transurethral resection of prostate
The procedure involves “reboring” of the central part of your prostate gland to improve the urine flow
TURP is one of the traditional procedure performed for BPH and most men get good relief of their symptoms
A catheter is used for a short time after the operation to wash out blood clots
The most common after-effects are the inability to emit semen during ejaculation and temporary bleeding, burning, or urinary frequency.
What does this procedure involve?
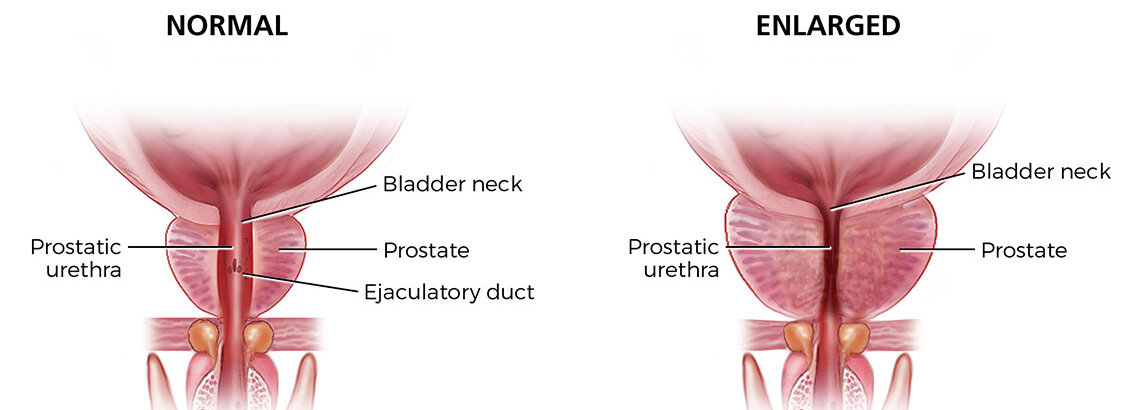
The prostate gland wraps around your urethra (waterpipe) as it leaves the bladder. As you get older, the prostate gland enlarges and it can block the flow of urine. TURP involves a cystoscopy (camera into the bladder) and removal of the obstructing portion of the prostate with electrical energy (diathermy). The goal is to create a wider prostate channel to allow the urine to flow more easily. Dr. Ashrafi will insert a temporary catheter into the bladder at the end of the operation. Bladder irrigations will continue for 1-2 days before the catheter is removed.
Enlarged Prostate Gland
Online Enquiry Form
What are the alternatives?
Observation (watchful waiting)
Medications to improve urine flow
Permanent catheterisation – especially in patients who, for any reason, are not considered suitable for surgery
Other surgical procedures
Robotic-assisted simple prostatectomy
The Urolift™ procedure
Rezum steam ablation
Laser prostatectomy
Prostate arterial embolisation (PAE)
What happens on the day of the procedure?
Dr. Ashrafi will meet with you and discuss the surgery again to confirm your consent. An anaesthetist will see you to discuss the options of a general anaesthetic or spinal anaesthetic. The nursing team will check your details and perform a safety checklist prior to your surgery.
Details of the procedure
We will do a final safety check
We will give you an injection of antibiotics before the procedure,
We put a cystoscope into your bladder through the urethra
We will remove (“shave”) the central portion of the prostate using electrical energy
The prostate is removed in small pieces preserving vital anatomical structures
The tissue is evacuated from the bladder
Once the prostate has been removed, we carefully cauterise any bleeding points in the prostate cavity
The prostate tissue will be sent for histopathology
A catheter will be inserted into your bladder at the end of the procedure
Bladder irrigation will be used in and out of the catheter to flush through any clots or bleeding
On average, the procedure takes between 45 & 60 minutes to complete
You should expect to be in hospital for one to three nights
We will remove your catheter at an appropriate time after the operation, usually between one day to one week afterwards.
After the catheter is removed, you may experience the following things
You may find it painful to pass urine at first
You may urinate more frequently than normal
You may feel you can’t hold the urine as well.
You may not be able to pass urine temporarily and another catheter may be inserted for a temporary period of time
You can have blood in the urine intermittently for up to 6 weeks
Are there any after-effects?
The possible after-effects and your risk of getting them are shown below. Some are self-limiting or reversible, but others are not.
Temporary mild burning, bleeding and frequent urination (almost all patients)
Retrograde ejaculation: no semen is produced because it passes back into your bladder on ejaculation (70%)
Treatment may not relieve all your symptoms (10-50%)
Bleeding requiring transfusion (5%)
Possible need to repeat the treatment at a later date due to re-growth of the prostate (2-10%)
Urethral stricture: narrowing of the urethra pipe (2-4%)
Bladder neck contracture: narrowing of the bladder and prostate junction (2-4%)
Inability to pass urine after surgery requiring a temporary catheter (2-10%)
Loss of urinary control which may be temporary or permanent (2-5%)
Finding incidental prostate cancer in the removed tissue which may need further treatment (2-10%)
TUR syndrome: irrigating fluid getting into the blood stream and causing confusion, heart problems and/or seizures (<2%)